Congenital Glaucoma
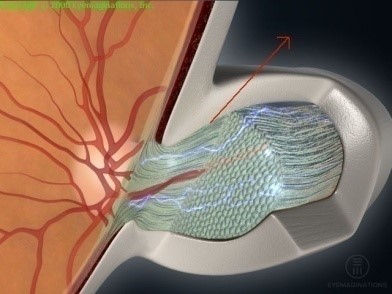
It is an elevated intraocular pressure due to drainage dysfunction of aqueous humor secreted by the ciliary body inside the eye. This causes accumulation of aqueous humor inside the eye, which leads to high intraocular pressure resulting damage to the optic nerve. It is congenital or occurs during first three four years of child age
Causes
- Occlusion or narrowing of the drainage opening.
- Eye infections may obstruct drainage channels
- Eye injury can damage the tissues of those channels.
Symptoms
- Abnormal corneal enlargement.
- Excessive tearing especially with exposure to flash light.
- Photophobia.
- Eye color changed to gray or pale blue.
Treatment
Important Tips
- Increased size or changed color of the infant cornea, require medical attention.
- Medication is very important to keep the intraocular pressures within normal level. Do not stop medication without doctor consultation.
- Medication helps maintaining normal intraocular pressure but not improving the vision
- Experience any vision acuity changes or side effects require medical consultation.